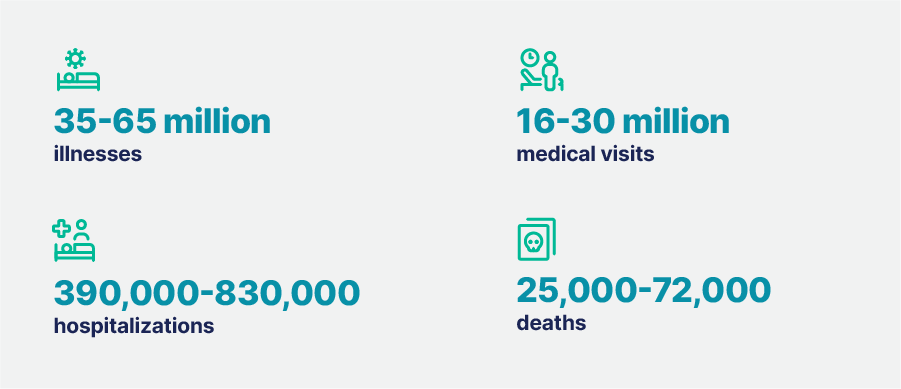
It’s that time of year again: flu season. It’s important to remember that the flu is still a serious public health concern. Every year, millions of people in the U.S. get sick from the flu, leading to thousands of hospitalizations and deaths. The Centers for Disease Control and Prevention (CDC) estimates that in the US, from October 2023 to June 2024, the flu resulted in:
Vaccination is considered one of the most cost-effective and safe methods to reduce flu illness and deaths. Despite this, vaccination rates remain low—only 48.5% of adults and 53.9% of kids got their flu shot in the 2023-2024 season.
So, why aren’t more people getting vaccinated, and what can be done to change that? Let’s break it down.
Why Some People Skip the Flu Shot
One of the biggest reasons people skip the flu shot is a lack of trust and knowledge about the vaccine. Some folks think the flu isn’t a big enough threat to bother with getting vaccinated, while others are skeptical about the safety and effectiveness of the vaccine itself. And let’s be honest, getting a shot every year because the flu virus keeps changing can feel like a hassle, especially if you’re already on the fence about it.
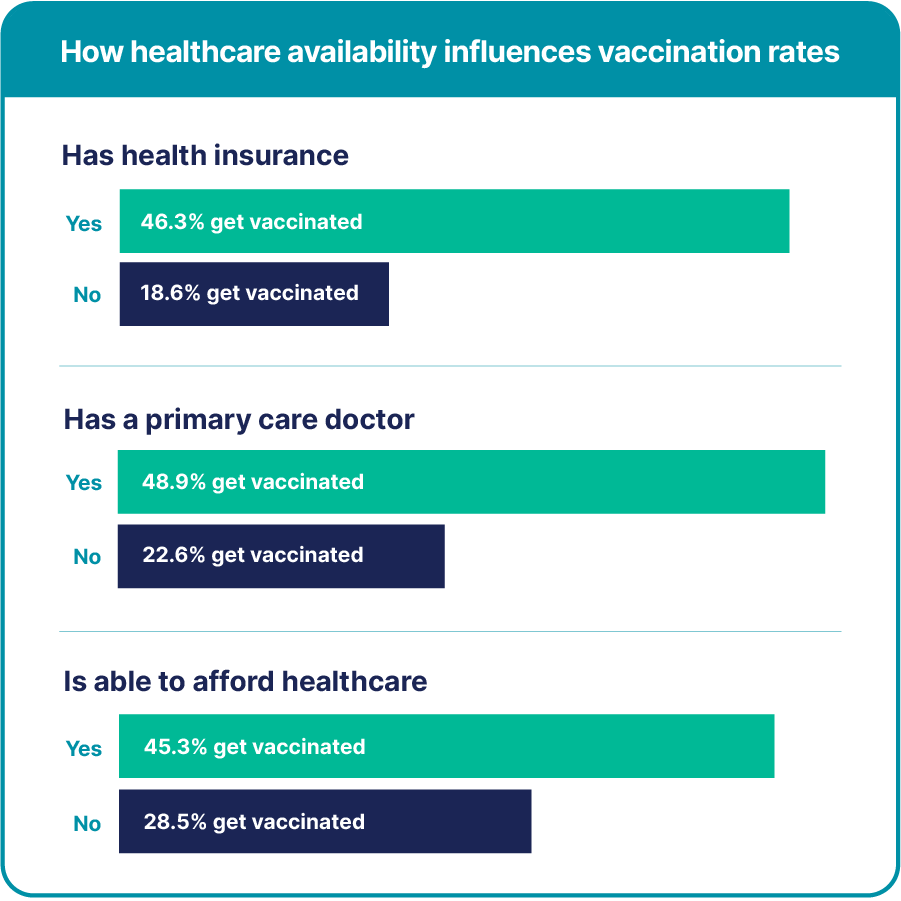
On top of that, there are barriers related to healthcare access. A recent study highlighted how having health insurance, a regular doctor, and being able to afford healthcare all play significant roles when someone is deciding whether or not to get their flu shot. If you don’t have these resources, getting vaccinated might feel like just one more inconvenience.
Unfortunately, these barriers mean that some groups are less likely to get vaccinated and are, therefore, more vulnerable to serious outcomes from the flu.
The Equity Issue
The issue of who gets vaccinated and who doesn’t isn’t just about personal choice or convenience—it’s also about equity. Social determinants of health (SDOH, like education, income, and housing, can affect people’s knowledge about and access to healthcare, including vaccines. For example, people with a college degree are twice as likely to get vaccinated as those who didn’t finish high school.
SODH have a profound impact on minority racial and ethnic groups. For instance, vaccination rates are lower among Black (36.7%), Hispanic (33.9%), American Indian/Alaskan Native (36.6%), and Native Hawaiian/Other Pacific Islander (37.9%) individuals when compared to White (46.5%) and Asian (44.1%) individuals. These gaps also show up in older adults on Medicare, making it clear that flu vaccination isn’t reaching everyone equally.
How Can We Improve Vaccination Rates?
So, what can be done to get more people vaccinated against the flu? There are a few strategies that can help overcome the barriers we’ve talked about.
First, clinical trials can play a significant role in improving access to vaccines. Since flu vaccination campaigns aren’t federally funded, states are left to decide whether to offer coverage programs for lower-income individuals, which can create a patchwork of availability. Clinical trials, especially those that provide vaccines at no cost to participants, can help fill in some of these gaps.
Another factor is trust. People are much more likely to get vaccinated if their doctor recommends it. That’s why it’s so crucial for healthcare providers to be knowledgeable about vaccines and to share that knowledge with their patients. At our research sites, we’ve seen success by building relationships with local doctors through lunch-and-learn educational sessions and office visits, which help keep them informed about vaccine trials and improve recruitment rates.
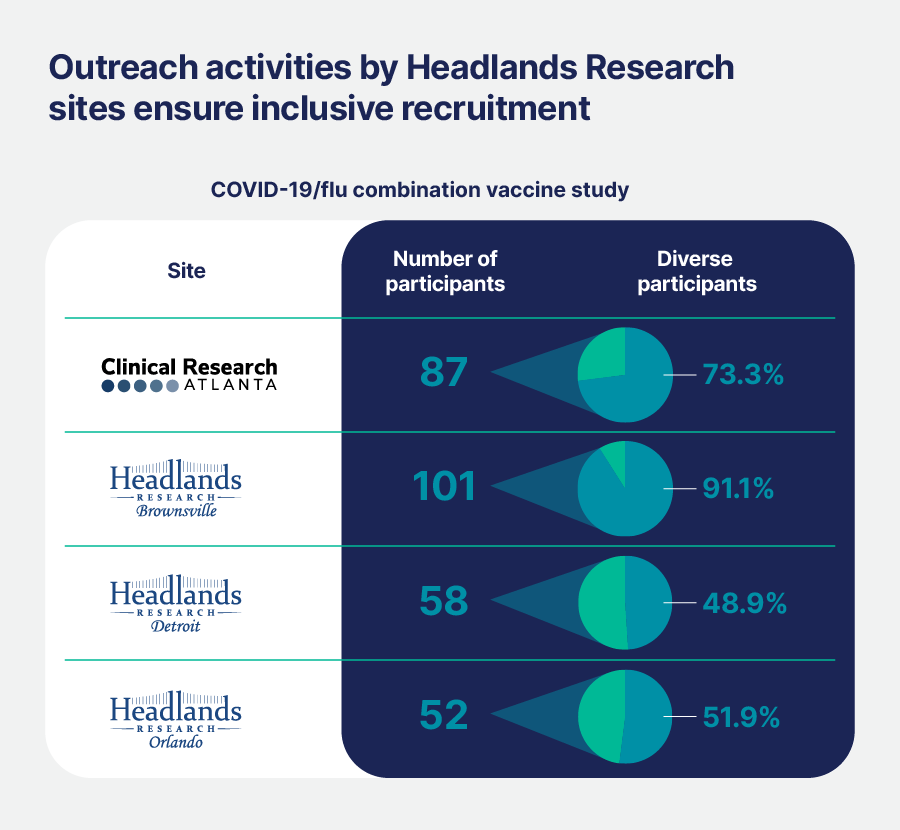
Making vaccines more convenient to get is another facilitator of vaccination. This could mean bringing vaccination services directly into communities through targeted outreach activities such as health fairs, educational sessions at community centers, or even mobile clinics. Younger adults, men, and people living in rural areas are among the least likely to get vaccinated, so finding ways to reach these groups where they are could make a big difference in public health.
At the same time, encouraging participation in vaccine trials among older adults, minority groups, and men could help address their long-standing under-representation in vaccine studies. Making it easier for people to get to study locations by providing transportation has also helped boost enrollment in our trials.
The Future: Combination Vaccines
One of the most exciting developments in vaccine research is the creation of combination vaccines that protect against multiple respiratory illnesses like the flu, respiratory syncytial virus (RSV), and COVID-19. To date, separate vaccines have been required. Combining them could make getting vaccinated easier and more convenient. However, some people are concerned about the safety and effectiveness of getting multiple vaccines at once, especially regarding potential side effects like arm pain, swelling, headaches, and fatigue.
Fortunately, clinical trials show that combination vaccines have significant advantages and can provide a strong immune response without increasing side effects compared to getting each vaccine separately. Plus, the convenience of a single shot for multiple illnesses could make it easier for more people to stay up-to-date on their vaccinations.
Partnering for Success
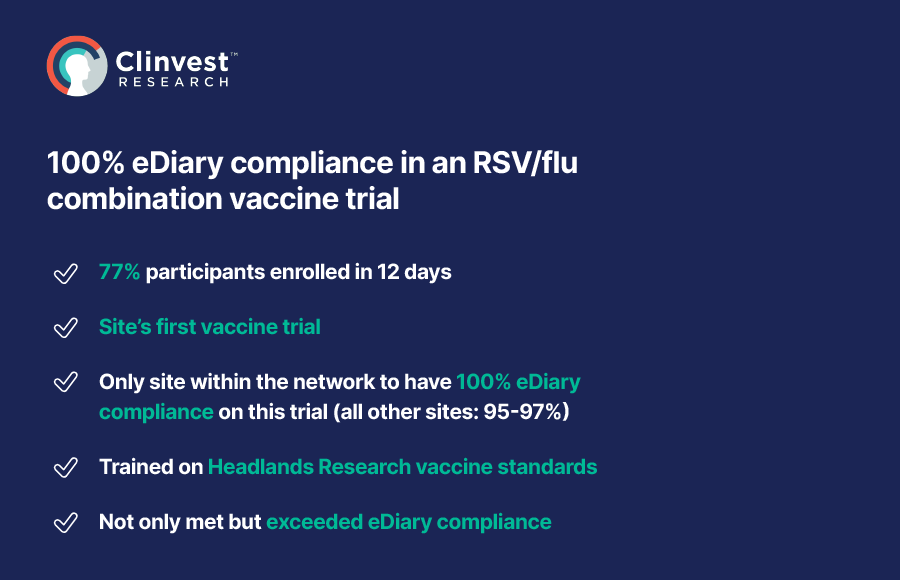
At the end of the day, improving vaccination rates is about more than just offering the shot—it’s about building trust, making vaccines accessible, and ensuring that everyone has the opportunity to protect themselves from the flu. Our network of 18 research sites across the United States and Canada has a proven track record of success in vaccine trials, with an overall 95% retention rate among participants. By focusing on participant engagement, working with Principal Investigators who reflect the communities they serve, and employing multilingual staff, we create a welcoming environment where people feel comfortable participating in and sticking with our trials.
As flu season approaches, it’s crucial to remember that vaccination is one of our best tools for staying healthy. Whether it’s through education, outreach, or innovative vaccine options, there are plenty of ways we can work together to ensure more people get the protection they need. Contact us to discuss how our sites can support your next vaccine trial.

