By: Dr. David Strong, Principal Investigator and Medical Director of Headlands Research Detroit, a Headlands Research site
As the two most common chronic respiratory diseases (CRDs) globally, asthma and chronic obstructive pulmonary disease (COPD) represent a significant burden for those affected as well as the healthcare system. Collectively, CRDs were the 6th leading cause of death in the U.S. in 2022, and individuals of working age with COPD are more likely to miss work than those without COPD. Similarly, asthma accounts for 14%-18% of absenteeism for school-aged children. As a result, the annual economic cost of asthma, including medical costs and loss of work and school days, is more than $81.9 billion, and the annual treatment costs for COPD in the U.S. are an estimated $50 billion.
The burden of asthma and COPD
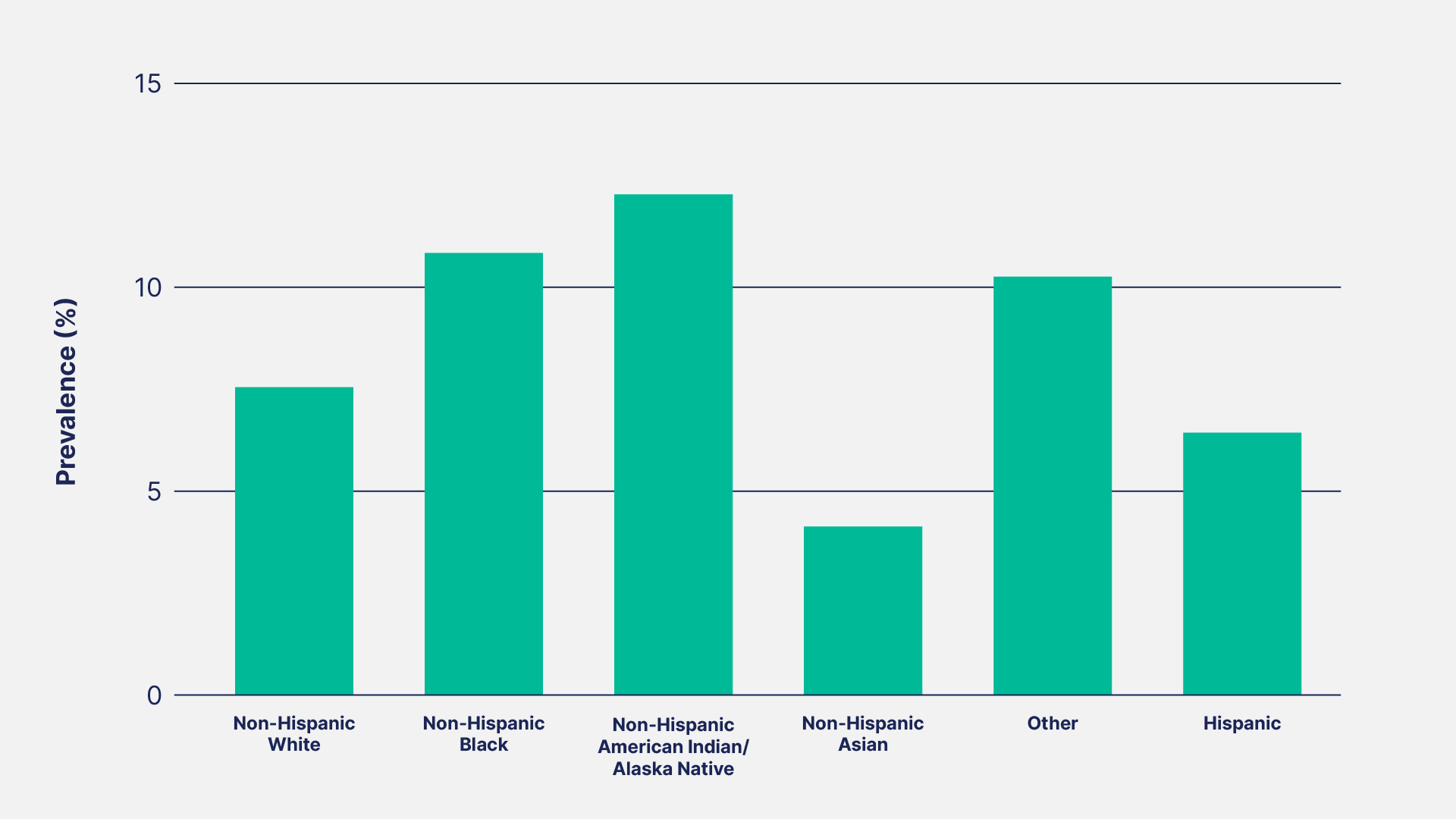
Asthma affects 7.7% of the U.S. population, including 6.5% of children and 8% of adults. It’s more common in females (8.9%) than in males (6.5%), and there are obvious disparities by race/ethnicity (see figure below).
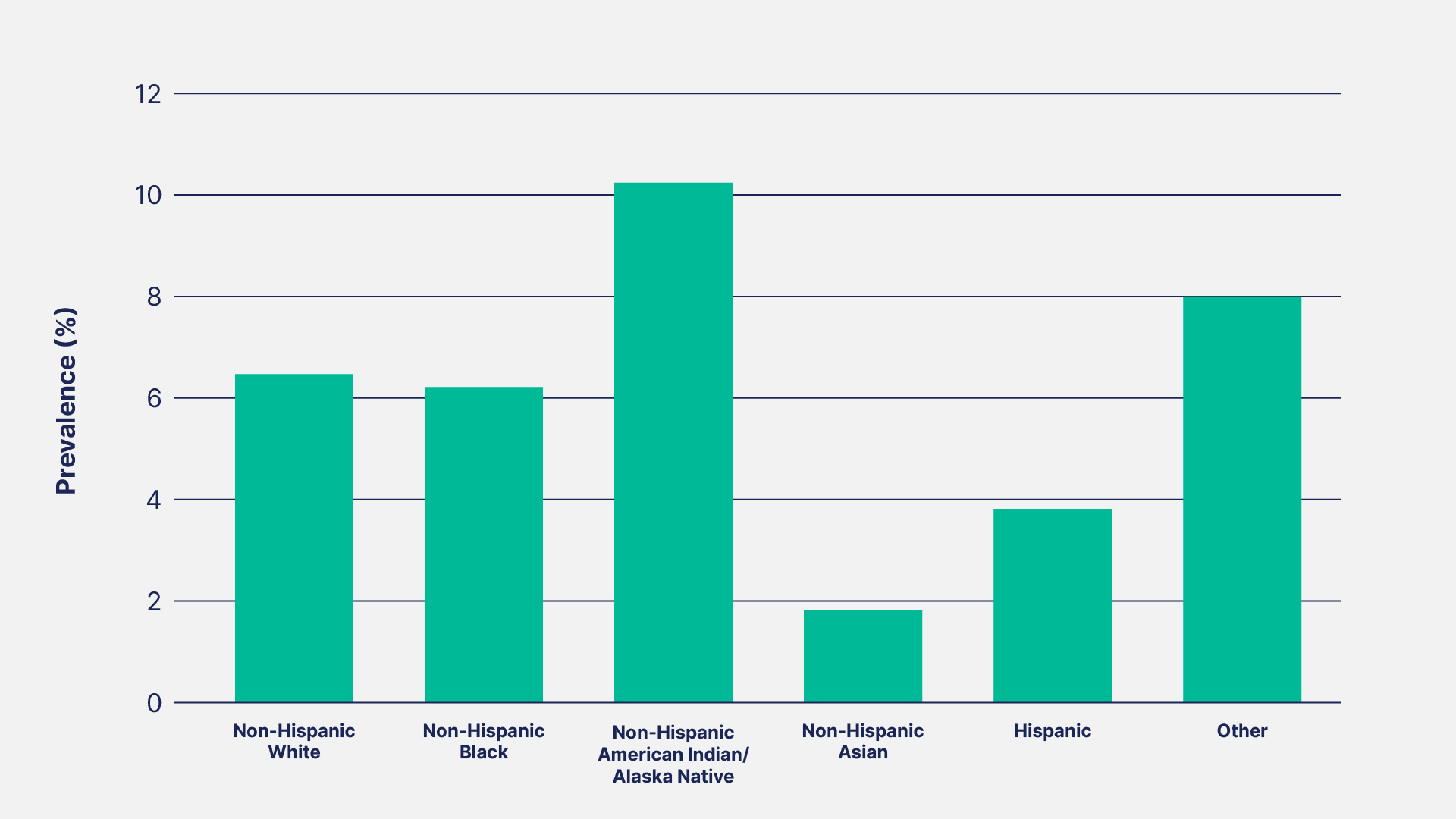
The prevalence of COPD in the U.S. adult population has remained stable at 6% overall for the past decade but has substantially increased for older adults (≥75 years), individuals in rural areas, and both current and previous smokers. However, one notable improvement is the decreasing prevalence in adults younger than 45 years old, potentially due to the decline in cigarette smoking in that age group. However, similar to asthma, disparities in COPD prevalence exist by race/ethnicity (see figure below).
The primary risk factors for these diseases, which involve the airways and other lung structures, are largely modifiable, including smoking (both first-hand and second-hand smoke), outdoor and indoor air pollution, occupational exposure, and overweight/obesity.
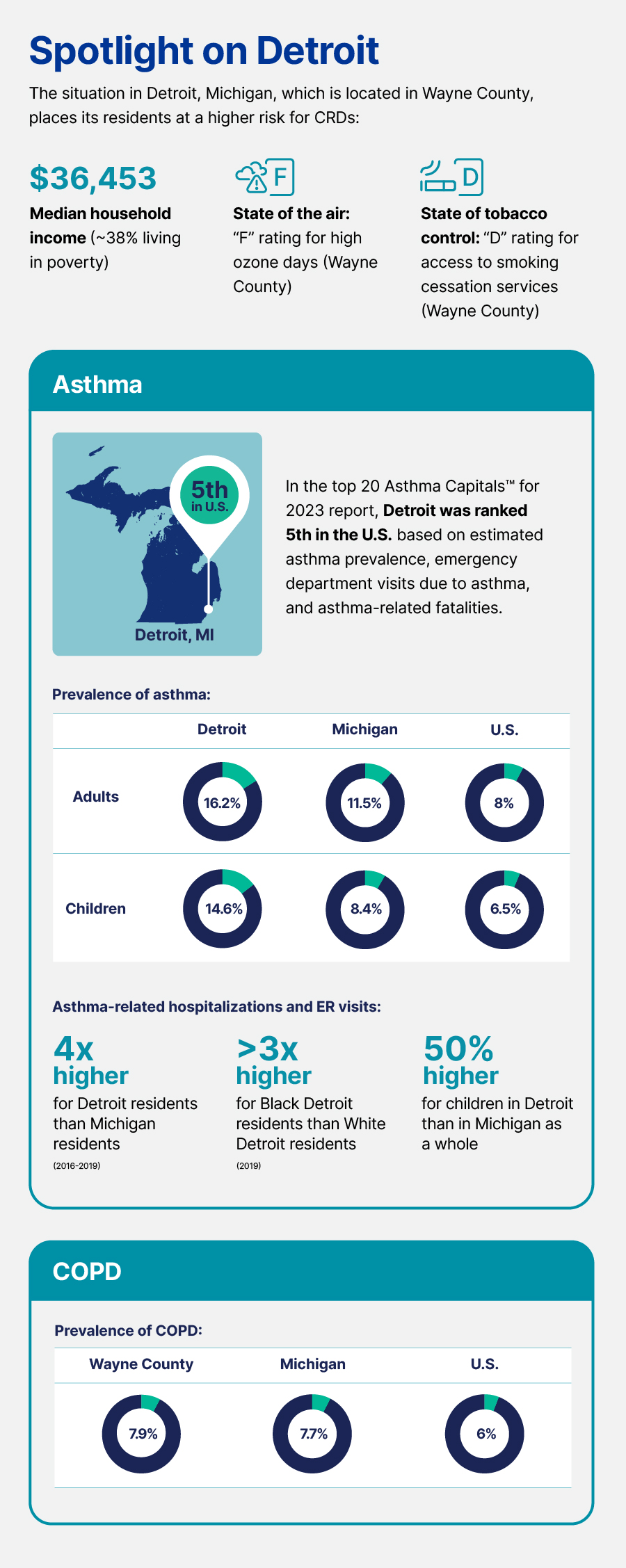
Lower socioeconomic status (SES) neighborhoods are known to have poorer air quality. This environmental risk, especially when combined with the greater occupational hazards for people of lower SES and limited access to healthcare in low-SES neighborhoods, contributes to higher rates of asthma and COPD. This is supported by the finding that asthma rates are highest, at 10.4%, for those living below the poverty line.
How asthma and COPD are treated
In asthma, the airways are inflamed and therefore narrower, which causes recurring periods of wheezing, shortness of breath, coughing, and chest tightness. The severity of these symptoms vary by person and can become worse during physical activity or at night. In contrast, COPD is caused by damage that blocks airflow, which also makes it difficult to breathe. Other symptoms include shortness of breath, chest tightness, and coughing, often with production of mucus. It’s a progressive disease, meaning its symptoms slowly worsen over time, resulting in greater impairment in activities of daily living.
There is no cure for either disease. Instead, the treatments focus on managing the symptoms by opening the air passages, reducing inflammation, and making it easier to breathe. These work well for some people, while others still struggle to keep their condition under control. Therefore, treatment typically needs to be closely managed by a healthcare professional, especially for COPD as it progresses.
Asthma is managed using both quick-relief medicines and drugs that provide long-term control. Inhaled short-acting beta2-agonists (SABAs) or anticholinergics help open the airways for immediate relief, while oral corticosteroids reduce inflammation in the air passages. Long-term control is achieved with corticosteroids as well as injected biologic medications, oral leukotriene modifiers, and inhaled mast cell stabilizers or long-acting bronchodilators (e.g., LABAs or LAMAs). Some of these are used in combination for the best asthma control. Other management strategies include avoiding exposure to triggers, such as smoke, fumes, dust, and pollen.
COPD is often managed in the same way as asthma using quick-relief medicines and medicines for long-term control. For severe COPD exacerbations that aren’t managed well, a phosphodiesterase-4 inhibitor may be used to decrease airway inflammation and relax the airways. Additional options for severe COPD include oxygen therapy, pulmonary rehabilitation, lung volume reduction therapy, and, in really severe cases, even lung transplantation. For smokers, stopping smoking is the most essential step in any treatment plan and can have a significant effect on disease progression and exacerbation.
Developments in asthma and COPD treatment
New treatments under investigation in clinical trials aim for better control with fewer side effects than the current treatment options.
For asthma, new medications that are under development are designed to reduce the number and potency of inflammatory cells and therefore minimize severe asthma exacerbations. Other medications may be able to completely block important inflammatory pathways completely.
In an exciting development for COPD, the U.S. Food and Drug Administration (FDA) recently approved a new inhaled medication with a unique mechanism of action for maintenance treatment of COPD. It’s the first inhaled drug with a new mechanism of action that has been approved for this indication in more than 20 years. It combines both a bronchodilator and an anti-inflammatory in a single drug that is inhaled directly into the lungs using a standard nebulizer. Drugs approved for other conditions are also being explored for their possible effectiveness in managing breathlessness in severe or very severe COPD.
Clinical research paving the way forward
The significant burden of asthma and COPD hinders quality of life for many individuals with these conditions. Although current treatments can be effective, many people with asthma or COPD still struggle to keep their condition under control, and the side effects of some medications can prevent their use. Clinical trials, like the studies being conducted at Headlands Research Detroit, are helping find better, effective treatments that can change the management of asthma and COPD in the future.

